It would be really nice if every time you called your veterinarian out for a lameness exam, it ended along the lines of, “Well, there you go. We’ve found out exactly what the problem is, and now we’ll just fix things up and your horse will be as good as new!”
By the way, I also think it would be nice if chocolate cake weren’t fattening; if the Arabs and the Israelis would spend their apparently boundless energies devising a wildly popular touring dance company, instead of focusing on less enjoyable endeavors; and if someone could come up with a soothing lullaby played on the accordion.
Anyway, the point is that this is the real world, and sometimes lameness diagnosis isn’t easy. It’s not like every horse has an obvious problem. So, when confronted with difficult cases, veterinarians will often recommend that he or she or someone use any one of several diagnostic machines in an effort to help pinpoint and identify the problem that’s making your horse limp. Here’s what to expect.
1) X-rays (or, if you like medical-speak, radiographs). X-rays are the oldest technology that veterinarians may use. X-rays are a form of electromagnetic radiation that were discovered in 1895 by Wilhelm Röntgen, a feat which won him the first Nobel Prize in physics. He called them X-rays because he didn’t know what the mysterious radiation was; the “X” stands for “unknown.” Known or not, they were immediately recognized as useful in medical imaging; they were used for that purpose within a month after Röntgen’s paper was published. In 2010, over 5 billion X-ray studies were performed.
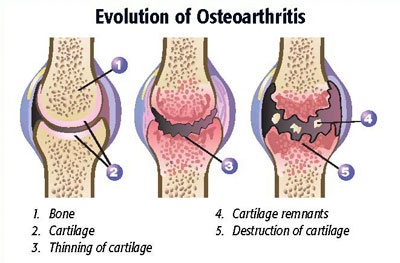
Anyway, X-rays are terrifically useful, especially for evaluating bone. To take an X-ray, your veterinarian puts a piece of X-ray film (or, in the case of digital X-rays, a plate with sensors in it) on one side of the limb, an X-ray camera on the other, and pulls the trigger. Any bones between the camera and the plate absorb most of the X-ray photons, because bones are more dense than soft tissue (bones have lots of minerals in them). Areas where there is less bone – say, tendons, joints, or even fractured areas – absorb less X-rays. The X-rays an image on the film or plate; when the film is developed, or when a computer analyses the plate, the parts of the image that received more X-ray exposure are dark, and those that got less (bones) leave a white shadow.
X-rays are great for looking at bones and joints. You can see the outline of bone bone, and the normal contour of joints. They are not nearly as useful at looking at soft tissue, however, since X-rays mostly pass right on through the soft tissue. There are certain techniques, called contrast radiography, where material that looks white on X-rays is injected into or around tissue. The white material shows up on the X-ray image, outlining or highlighting the area examined. That’s not something that you’re going to see very often in routine lameness diagnosis, however.
2) Scintigraphy. Also known as a “bone scan,” scintigraphy takes advantage of the process of inflammation to try to localize an injured area.
When an area is inflamed, blood vessels get “leaky,” and allow fluid to seep out of them (that’s one reason why injured tissue swells). Scintigraphy uses a radioactive substance that is injected into the horse’s bloodstream. The radioactive substance follows the fluid, and also “leaks” into inflamed areas. The increased radioactivity in a particular area can be picked up with a counting device and, voilà, you’ve got a “bone scan.”
Scintigraphy has the advantage of being pretty sensitive, that is, it’s pretty good at picking up areas of inflammation. However, it’s not very specific, that is, it doesn’t usually tell you exactly what structure is inflamed. Bone scans aren’t particularly difficult to perform, but they do require special equipment, so they aren’t available everywhere. Plus, the horse examined with a bone scan has to be held in a special area until he’s no longer radioactive (about 24 hours).
3) Ultrasound– Ultrasound has been used to image human bodies for half a century, and has been applied to horses since the early 1980’s. Ultrasound waves are sound waves that are higher than those that can be heard by humans; the ultrasound sound beam is used to evaluate primarily soft tissues in the horse’s limbs, mostly the tendons and ligaments of the lower limb, but also some joints and cartilage surfaces. Of course, ultrasound machines are also tremendously useful for evaluation of structures of the horse’s reproductive system – no reproductive medicine specialist would be without one! In fact, just about anything that’s swollen can be evaluated with an ultrasound machine, if need be.
Ultrasound waves penetrate the soft tissue, and bounce back. The reflection of the waves can be measured, and the signal transformed by a computer into a grey-and-white image that you can see immediately.
4) CT (Cat Scan; Computed Tomography) – CT is a combination of a computer and X-rays. CT takes a whole bunch of conventional X-rays, rotating around an axis. The computer takes all of these images, and using a process known as digital geometry processing, generates a 3D image. As such, you can get some very detailed images of areas that are rather difficult to image with plain X-rays (such as the foot).
As fun as CT is, and as pretty as the pictures are, the equipment is very expensive, and access to the machine is pretty limited, so it’s not widely used, certainly not as widely as other imaging methods.
5) MRI (Magnetic Resonance Imaging) – MRI has been available for only about the past decade or so. It’s use has allowed veterinarians to see things that they hadn’t seen before. In fact, this has been something of a problem, since it’s taken a while to figure out what’s normal when you take an MRI of a horse.
An MRI machine uses a powerful magnetic field and pulses of radio waves to produce detailed images of the horse’s body. Unlike CT scans or X-rays, MRI provides good contrast to the soft tissues of the horse’s body, making it particularly useful in sorting out problems in the complicated anatomy of the horse’s hoof. It can be used in many locations on the horse’s body, although it’s certainly not cheap.
6) Thermography- Thermography is, without question, the imaging modality that generates the prettiest pictures. It’s also the one modality that has not been generally accepted by the medical community, human or veterinary. That is, the images don’t seem to be reliable indicators of any problem, or, they might give you a pretty picture of a problem that you already knew was there. It’s been around for a couple of decades, with still no real consensus on usefulness, so it’s probably not an imaging method that you should hang your hat on. It’s also subject to lots of variables like wind currents – even those that are really faint. Those who like (or promote) the modality seem to like it a lot – others, not so much.
Of course, each and every image that you take comes at a cost, but that cost can often be worth it if the information that you get can help set up an effective treatment plan, or help give a more accurate prognosis. But here’s the thing – diagnostic imaging should never be a substitute for a thorough lameness exam. Diagnostic machines can be very helpful, but don’t forget to look at the horse!